Myofascial Therapy
Myofascial Trigger Point Therapy - What Is It?
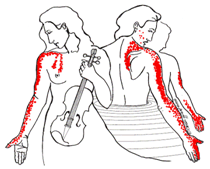
Illustrations of Trapezius and Scalene trigger point referred patterns by C.M. Shifflett (at the top).
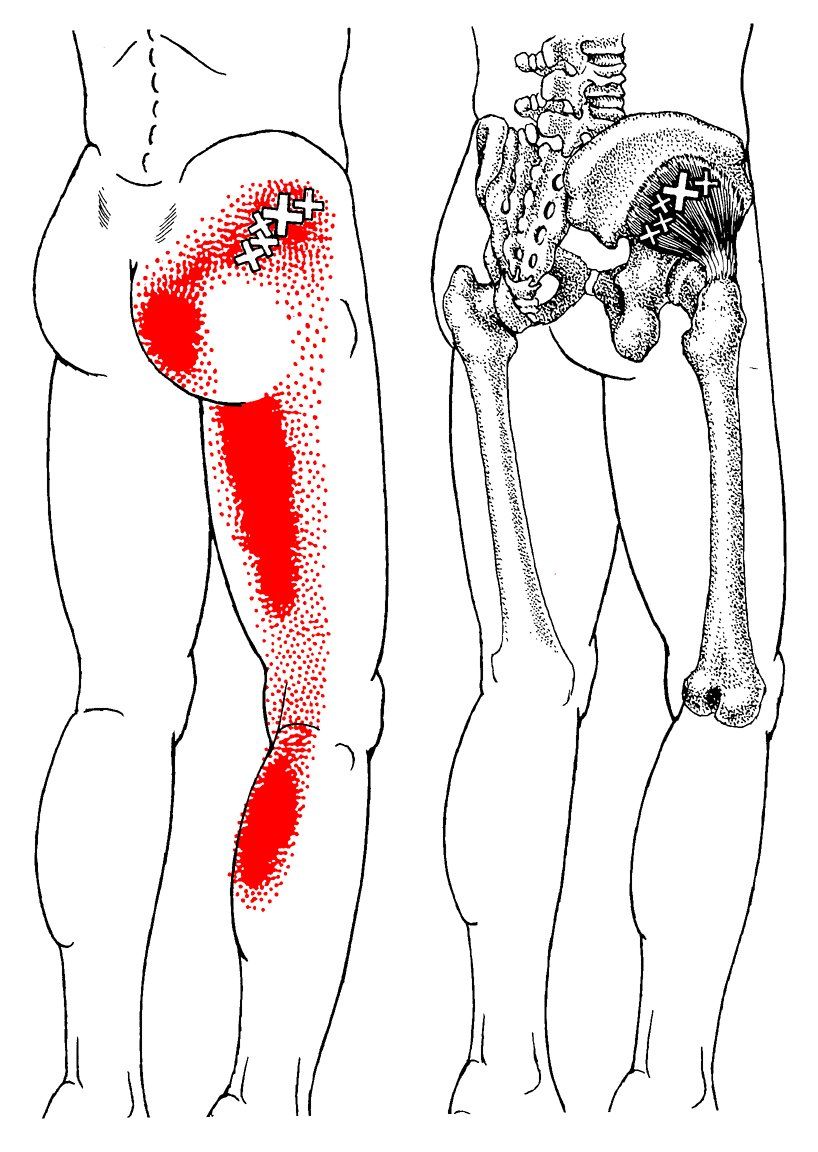
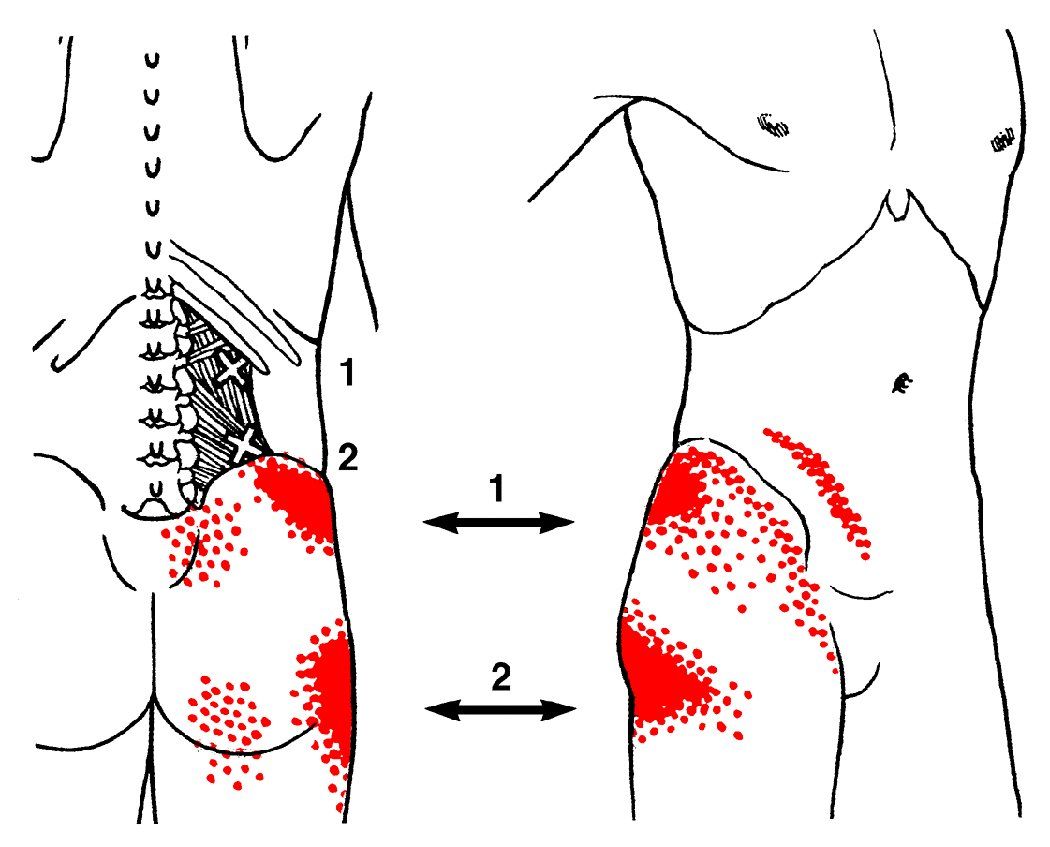
Illustration of Gluteus Minimus and QL trigger point referral patterns by Barbara D. Cummings (Lower)
Myofascial Pain and Trigger Points: Getting to the Point
Myofascial trigger points are an extremely common cause of pain. Trigger points are painful when pressed on, cause a shortening of the muscle fibers, and have a special property called referred pain. However we now know that the referred phenomenon can be felt in many ways including sensation like; tingling, numbness, pain, dull aching or shooting pain. Referred sensation means that a trigger point in one muscle can create a sensation or pain into another , sometimes distant area.
For instance, when the muscle at the top of your shoulder (trapezius) has a trigger point it will refer sensation up the side of your neck and head causing a headache. Active myofascial trigger points in the muscles of the shoulder neck and face are a common source of headaches. In many instances the headache has the features of so-called "tension headache", but there is increasing acceptance that myofascial trigger points can initiate classical migraine headaches or be part of a mixed tension/migraine headache complex.
- Back pain
- Headaches
- Neck pain
- Rotator cuff (shoulder) pain
- Jaw pain (TMJD)
- Tennis elbow
- Carpal tunnel syndrome
- Hand and arm pain
- Repetitive Strain Injuries
- Pelvic pain
- Hip pain
- "Sciatic" pain (buttock and leg pain)
- Leg and knee pain
- Plantar fasciitis (foot) pain
- Tendinitis/tendinopathy
- Burstitis
- Arthritis
- Disc pain (bulge/rupture/herniation) and radiculopathy
- Frozen shoulder
- Fibromyalgia
- and MUCH more
Muscles have been an under-treated cause of pain. In fact, with a specialized area of medicine for almost every area of the body (heart, eyes, lungs, intestines, kidneys, etc), oddly, there is no muscle specialty in medicine. Myofascial pain from trigger points is often over-looked as a possible source of pain by those seeking relief.
Unfortunately, common though the condition may be, the diagnoses and treatment of Myofascial Pain has yet to be included in most medical training. The majority of patients seeking relief from pain are still treated with the traditional approach of anti-inflammatory medications, muscle relaxants, anti depressant medications and/or strengthening programs. These prove ineffective, if not detrimental, as trigger points do not respond to them and may be aggravated by further straining (strengthening exercises). Currently there is no evidence that any form of drug treatment eliminates myofascial trigger points. NSAIDs and other analgesics usually provide moderate but very temporary symptomatic relief.
It is encouraging that myofascial trigger points are becoming more commonly considered when physicians diagnose their patients. Some primary care physicians, regularly administer trigger point injections. Some medical providers recognize the presence of trigger points and refer their patients for treatment by Myofascial Trigger Point Therapists. This creates best clinical outcomes.
Research on Trigger Points
How Trigger Points are Formed
- Repetitive overuse injuries (using the same body parts in the same way hundreds of times on a daily basis) from activities such as typing/mousing, handheld electronics, gardening, home improvement projects, work environments, etc.
- Sustained loading as with heavy lifting, carrying babies, briefcases, boxes, wearing body armor or lifting bedridden patients.
- Habitually poor posture due to our sedentary lifestyles, de-conditioning and poorly designed furniture
- Muscle clenching and tensing due to mental/emotional stress.
- Direct injury such as a blow, strain, break, twist or tear. Think car accidents, sports injuries, falling down stairs and the like.
- Surprisingly, trigger points can even develop due to inactivity such as prolonged bed rest or sitting.
- The damage to muscle and connective tissue which results in trigger points can occur several ways. It can happen as the result of:
- Surprisingly, trigger points can even develop due to inactivity such as prolonged bed rest or sitting.
Active Trigger Points Cause Pain
Latent Trigger Points Matter Too
- Restricted movement
- Distorted muscle movement patterns
- Stiffness and weakness of the affected muscle
How Many Trigger Points Can I Have?
Establishing if Trigger Points Are Present
"You cannot strengthen a muscle that has a trigger point, because the muscle is already physiologically contracted. Too many physical therapists see a weakened muscle and immediately attempt to strengthen it without testing for the presence of trigger points. Attempts at strengthening a muscle with trigger points will only cause the trigger points to worsen..."
— Devin Starlanyl, MD author of Fibromyalgia and Chronic Myofascial Pain Syndrome: A Survivor's Manual
What to Expect from Treatment
- Type of injury and length of time since it occurred.
- Overall physical health and level of fitness
- Perpetuating factors (many can be eliminated, others can not)
- Underlying skeletal abnormalities
- Nutrition (vitamin and mineral deficiencies, poor diet etc.)
- Quality of sleep
- Depression or anxiety
- Patient compliance with self-care and eliminating or reducing perpetuating factors.
- Other medical conditions (i.e. allergies, diabetes, thyroid dysfunction, etc.)
- Take a full medical and pain history
- Evaluate your pain map for referred pain patterns
- Assess the ergonomics of your work station and other regular activities.
- Assess and make suggestions to improve the quality of your sleep
- Make nutritional recommendations based on lab results from your physician ordered blood work or refer you to a qualified health care profesional to assist you with this.
- Make suggestions how to choose an appropriate exercise/movement program and help you to encorporate it into your life.
- Help you to learn some self-treatment, self management and self care to assist you to treat your condition and your trigger points. The degree that self care will help can depend on many factors including how complex the condition is, if perpetuating factors can be eliminated, your dedication to the self care/making changes and many others.
Get Treatment from a trained practitioner now:
Locate a Myofascial TherapistTreatment goals will be developed together with your myofascial trigger point therapist. Assessment of key perpetuating factors, muscles that are contributing to your problem will be identified and treatment techniques will be applied. Your input and insight are highly encouraged.
Pictured here: Tasso Spanos, NAMTPT 2015 Lifetime Achievement Award Recipient, demonstrates a treatment technique stretching the hamstrings.